You can now find our latest updates at https://scharr.dept.shef.ac.uk/publichealthtopics/
Discussing ‘Tricky Topics’ with Young People at a Distance: the Challenges of Exploring Sensitive Subjects in Virtual Focus Groups
Covid Realities is a research project looking into the experiences of parents and carers on low incomes during the pandemic. Dr Nick Woodrow, Research Associate in ScHARR has written a blog which features on their site. https://covidrealities.org/researching-poverty/tricky-topics-young-people
Filed under Uncategorized
The Practice and Research Collaborative (PaRC) Yorkshire Humber: Two years on
In June 2021, the Practice and Research Collaborative (PaRC) Yorkshire Humber will celebrate its second anniversary (https://youtu.be/yQs6uMRvENc). PaRC is led by Professor Liddy Goyder and managed by Dr Annette Haywood (ScHARR) and is a conduit for public health research and knowledge exchange across the Yorkshire and Humber Region. Its mission is to integrate public health research and practice by building on existing national and regional public health structures. PaRC is a way of bridging the research into practice gap and linking academic institutions with local authority based public health practitioners to enable collaboration on research that can translate into the provision of improved public health practice through evidence based interventions.
We have established a successful management group comprising representatives from our academic partners, research interested colleagues within local authorities, public health registrars, Public Health England, and the NIHR Clinical Research Network. PaRC is funded from a number of sources including legacy funding CLAHRC (South Yorkshire and Yorkshire Humber); CRN and PHE. We are able to showcase a variety of activities from our inception in June 2019, including successful funding applications, supporting applications from our local authority partners, developing networks (e.g. Yorkshire Obesity Research Alliance; YORA – https://www.parc-hub.co.uk/links-and-resources/yorkshire-and-humber-obesity-research-alliance-yora/), forging partnerships with our academic institutions, supporting fellowships (https://www.sheffield.ac.uk/scharr/people/staff/alexis-foster) and ensuring close linkages with existing infrastructure, including NIHR Public Health Research Applications and Design Advice – PHRADA (https://www.rds-yh.nihr.ac.uk/wp-content/uploads/2020/09/RDS-PHRADA-what-we-do.pdf). We are also supporting a number of workshops across the region which aim to develop the skills of the public health workforce.
Contact details:
Dr Annette Haywood, Manager Public Health Practice and Research Collaborative (PaRC) YH, School of Health and Related Research
Email: a.haywood@sheffield.ac.uk
Follow us on Twitter! @ScHARRPubHealth @annettehaywood @PaRC_YH
Filed under Uncategorized
An Undergrad’s experience of the Think Ahead SURE Scheme
This summer I was lucky enough to take part in the Think Ahead SURE scheme, a summer research programme lasting for 6-8 weeks at the University of Sheffield based in the Faculties of Medicine, Dentistry and Health or Science. Prior to application, prospective applicants are able to review the wide variety of projects available to work on and apply to several simultaneously. Each project is designed and headed by a PhD student who supervises the undergraduate, providing a unique opportunity for peer learning and research. The application process is competitive requiring the submission of a CV and covering letter followed by a panel interview headed by the project leaders.
The Project and its context
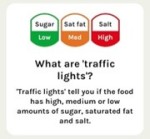
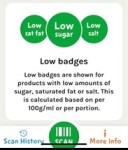
 The Project I worked on was offered by a PhD student in ScHARR and aimed to map out the Behavioural Change Techniques (BCTs) of the Change4Life Food Scanner app. Behavioural Change Techniques are the ‘active ingredients’ of evidenced-based behavioural strategies. These include things like social support, prompts and ques and feedback on behaviour to name a few. The app itself was developed by Public Health England as part of a wider public health campaign aimed at families to target obesity. The app works by allowing the user to scan the barcode of food products and then provides the nutritional content of the item presented in several ways. Evidence suggests that interventions with a theoretical grounding tend to be more successful in achieving their intended outcome, however it was unclear whether the Change4Life Food Scanner app was designed with theory in mind. BCT mapping was therefore required to identify the presence of BCTs, and their combinations, in order to provide a basis for evaluation of the intervention. The project mapped an updated and outdated version of the app finding that both encompassed BCTs which have previously been found to be effective in similar settings.
The Project I worked on was offered by a PhD student in ScHARR and aimed to map out the Behavioural Change Techniques (BCTs) of the Change4Life Food Scanner app. Behavioural Change Techniques are the ‘active ingredients’ of evidenced-based behavioural strategies. These include things like social support, prompts and ques and feedback on behaviour to name a few. The app itself was developed by Public Health England as part of a wider public health campaign aimed at families to target obesity. The app works by allowing the user to scan the barcode of food products and then provides the nutritional content of the item presented in several ways. Evidence suggests that interventions with a theoretical grounding tend to be more successful in achieving their intended outcome, however it was unclear whether the Change4Life Food Scanner app was designed with theory in mind. BCT mapping was therefore required to identify the presence of BCTs, and their combinations, in order to provide a basis for evaluation of the intervention. The project mapped an updated and outdated version of the app finding that both encompassed BCTs which have previously been found to be effective in similar settings.
My Experience
Undertaking this project has helped me develop both academically and personally.
One of my preparatory tasks was to prepare a grant application to fund the research project. Having prepared the application along with my supervisor, we were about to submit when we were informed that the organisation we were applying to were cancelling funding due to Covid-19. Further bad news followed when we were informed by the University that due to the impending Lockdown and the Covid-19 pandemic, the SURE scheme would be cancelled this year. This was devastating; however, both my supervisor and I were determined not to lose the opportunity. Together we negotiated with the organisers of the scheme to allow us to continue with the project. This meant that we had no funding, we would be working from home on a voluntary basis and I would be undertaking the project part-time while working a part-time job. This taught me determination, perseverance and time management skills. The project allowed me to experience the inner workings of academic research from literature searches and presenting results to preparing a manuscript for publication which has ignited a desire to pursue further research activities and has equipped me with invaluable experience which I hope to apply in my future study and career. At present, our manuscript is being reviewed for publication and should it be accepted, would mean that I will be a second author on a published piece of research as an undergraduate – something which I never would have imagined happening!
A Call for ScHARR Students
While the SURE scheme is open to PhD students and early career researchers from the Faculties of Medicine, Dentistry and Health or Science, there are very few projects offered by ScHARR. I would therefore encourage any PhD students and early career researchers from ScHARR to get involved with the SURE scheme, providing a greater variety of projects for the undergraduate students to get involved with. The SURE scheme is a fantastic opportunity for PhD students and researchers to gain supervisor experience and help an undergraduate flourish in their own research experience.
Emily Michalik-Denny
Filed under Uncategorized
Organising virtual conferences during the COVID-19 pandemic
This year, I was on the organising committee for the Early Career Alcohol Research Symposium (ECARS) and the Society for the Study of Addiction (SSA) PhD Symposium. Both would initially take place in-person, but it quickly became clear that this was not possible this year. We thought it was important to try to organise online replacements, as conferences are great opportunities for early career researchers (ECR) and PhD students to present their work and network. In this blog, I will reflect on my experience organising and participating in these virtual conferences and I hope this will helpful for those who are planning virtual conferences in the future.
Accessibility
The main advantage of running our events online was increased accessibility. Both ECARS and the SSA PhD Symposium would have been able to accommodate a maximum of 40 delegates in person. However, more than 80 delegates registered for both events and we could accommodate them all online. Many of them would not have been able to attend face-to-face as they were from outside the UK, had other obligations, or did not receive funding for conference travel. Delegate feedback for both events showed that these delegates especially valued the opportunity to present their work and/or network with their peers.
The same benefits applied to external speakers. Both of our events included a career advice panel. Because speakers did not have to travel all over the country for a one-hour session, we could invite a wide range of panel members, including people from outside academia and someone who was on maternity leave at that time. Their perspectives were very useful for delegates and it would have been more challenging to arrange this face to face.
Finally, as a conference attendee myself, I noticed that the online format appeared to encourage ECRs to ask more questions and get more involved in the discussion than in previous conferences.
Logistics
We used Blackboard Collaborate for ECARS and Zoom for the SSA PhD Symposium, because we had institutional licenses for these. Technical difficulties were our biggest concern, as there is little you can do when speakers have weak internet connections or are unable to log in. Luckily, at both events we only had technical problems for one or two speakers, and everyone else was able to do their presentation without trouble.
Blackboard and Zoom had their advantages and disadvantages. Blackboard allowed us to upload the presentations to the meeting in advance, so we didn’t need to rely on speakers to share their own screen (which may be difficult for speakers with poor internet connections). However, that also meant speakers couldn’t use transitions or animations in their PowerPoint slides. In Zoom, speakers had to share their own screen in order to give their presentation. This wasn’t possible for some speakers, which meant that the chair had to share the presentation on their own screen instead. Most delegates were already familiar with Zoom and everyone was able to join, whereas some delegates were not able to access the Blackboard meeting due to it being blocked by their firewall. Zoom also allows you to see multiple videos at once, which was great for socialising during breaks, whereas on blackboard you can only see 6 videos at once. On the other hand, Blackboard has a built-in “raise hand” functionality, which made chairing Q&As much easier, which was lacking on Zoom. For future events, it is worth investigating different conference platforms to find one that matches your requirements.
Socialising
Networking and socialising are important reasons to attend conferences for many people. This was one of the most challenging things to try to implement online. We encouraged delegates to turn on their audio and video during breaks to get to know each other and/or use the chat function to socialise. However, it is hard to hold a conversation online with large groups. At ECARS, we scheduled breakout discussions at the end of each session, which allowed delegates to get to know each other in smaller groups. However, connecting to breakout groups in Blackboard takes quite a long time and this caused some delegates to drop out of the session. At both events, we organised a social event (game/quiz) in the evening to try to replace the conference dinner. Whilst delegates told us they wanted more opportunity to connect with each other, very few attended the evening event. It seems that after a day of online sessions, delegates do not want to spend their evening online too. Future online conferences may want to consider opening a “socialising room” where delegates can drop in and out at different points in the conference to meet others.
Overall, there are many benefits to running an online conference and organisers can choose a platform that suits their needs. Given that we all need to reduce our carbon footprint and that online conferences are accessible to a wider audience, it would worth considering online options for future events even after the pandemic is over.
Dr Inge Kersbergen
SSA Research Fellow, School of Health and Related Research
Filed under Uncategorized
Learning from a School Streets pilot in Sheffield: Creating healthy community spaces in a time of COVID-19? – Dr Amy Barnes
Sheffield Schools Carterknowle Junior and Holt House Infants released a community-led evaluation report on 8th October 2020 (Clean Air Day!) about their week-long ‘School Streets’ pilot in late 2019, which involved closing part of Bannerdale Road in the city. I worked with the school community on the pilot and we have learned a lot together.
‘School Streets’ have been trialled across the country. They involve restricting car access near schools during drop-off and pick-up to make streets healthier and safer for children. They often involve other local action too: encouraging active travel, ‘citizen science’ activities to get people involved in monitoring air quality or traffic flows, and organising events so that the community can celebrate and enjoy the space created.
During the closure, we found that 4 out of 5 families opted for active travel, by walking, cycling or scooting to get to school. The report looks at changes in air quality and traffic volumes during the road closure. It also explores the views of parents, children and local residents.
By working together, we learned that School Streets can create a new local space for children and families: to play, interact, feel safe, be active and be independent. As a local resident, quoted in the report, said:
“There were some teething problems on the first day but once people who use the road were aware of the closure, there was a real difference around the peak hours. The road was not only quieter, but it also felt more open and calmer.”
Our report shows that there is a lot of support locally for more action to create School Streets. The pilot was not without its issues and these are also discussed in our report. For example, the impact of closing the road displaced some of the remaining commuter traffic onto nearby roads, increasing congestion there.
In terms of air quality, we worked with Dr Maria Val Martin, an atmospheric scientist at the University, who was involved with monitoring air quality during the closure. As Maria explained:
“The results from the air quality sensors during the plot week were inconclusive. We’d need a much longer period of time to show if there’s a sustained impact on air pollution reductions. However, we know from NO2 readings during the 2020 lockdown that the reduced traffic resulted in consistently lower NO2 levels compared to the averages from 2016-19.”
In the midst of this global COVID-19 pandemic, perhaps now more than ever people need cleaner air to breathe and safer outdoor community spaces to help with physical distancing. ‘School Streets’ schemes could have a vital role to play here. We want all Sheffield and city communities to have the resources to take action to create safe and healthy School Streets as we deal with COVID-19. This will require bold city leadership but we are confident that Sheffield and other cities can seize the opportunity to make ‘School Streets’ schemes a reality.
If you agree, lets start a conversation about it…
Dr Amy Barnes, Lecturer in Public Health (Policy)
Email: a.barnes@sheffield.a.uk
Dr Maria Val Martin, University of Sheffield
Nikki Rees, Co-opted School Governor
For more information about the pilot, you can also Jenny Johnson, Parent Governor, Holt House & Carterknowle Schools Federation.
Filed under Uncategorized
Supporting ScHARR’s teaching for 2020-21
After the emergency responses needed for the continued delivery and assessment across our programmes since late March, responding to the COVID-19 pandemic lockdown, we are now busy preparing for the start of the 2020-21 academic year with some significant challenges and opportunities to keep us on our toes. We are all sad to see the departure of Rosalyn Ferguson, whose skilful leadership has shaped ScHARR’s vision for consolidation and redevelopment of our Masters-level courses in response to the University’s Programme Level Approach (PLA) initiative. A significant challenge will be to maintain momentum for our PLA developments and it is helpful that UEB has revised the PLA roadmap to allow more time for consideration of how better to embed employability, inclusivity and sustainability in our programmes at a time when we are all focusing on adapting our delivery of teaching and assessment for next semester. In the past few weeks, we have seen a number of changes in module leadership and a strong response from all quarters of ScHARR – academic, research, professional services and administrative staff alike. To ensure that we are well placed to respond flexibly to either a need for tighter restrictions on or more open access to campus-based teaching, essential for good student experience. While there is still some uncertainty about how our teaching will look across the semester, to help prepare for 2020 Luke Miller, Rosalyn Ferguson and Peter Grabowski are delivering a series of three ‘Bytesize’ sessions. Focusing on considerations for developing alternative assessments to replace timed invigilated exams, resources available for engaging students actively in synchronous and asynchronous delivery of learning outcomes, improving the accessibility of learning resources for students in line with recent changes in legislation, and keeping PLA priorities in mind as we go forward.
Learning and Teaching Publication
Rosario E, Grabowski P, Evans M. (2020). How do spaces for learning and teaching impact upon the achievement of small group learning outcomes? A student perspective at the University of Sheffield, UK. Student Engagement in Higher Education Journal. 3(1):157-166
In this project, funded by the Student Engagement team at the University of Sheffield, a group of six Student Ambassadors for Learning and Teaching (SALT), drawn from across the Faculty of Medicine Dentistry and Health, developed a questionnaire to assess student views of the appropriateness of current teaching and learning spaces for achieving target learning outcomes across small group learning activities. In follow-up focus groups, they further explored how a range of teaching spaces might impact upon the achievement of learning outcomes. Drawing also from the literature, they looked beyond environmental factors (lighting, heating, noise etc) to identify three key recommendations that could be easily adopted, for Faculty to consider when planning the reconfiguration of learning spaces; easily configurable rooms for the flexibility to work in different group sizes, multiple visual aids to encourage better engagement and more innovative spaces with dynamic layouts that help regulate the power balances among teachers and learners and that encourage participation. Impacting beyond the Faculty, the University’s central Learning, Infrastructure and Space Management Group endorsed the SALT recommendations, agreed that they should inform the University’s current refurbishment programme for learning and teaching spaces and agreed that student views should be included in refurbishment planning going forward. The paper includes reflections on the project from the SALT Lead (ER), the academic supervisor (PG) and the L&T Professional Services supervisor (ME) and it demonstrates effective empowerment of students’ voice across the Faculty.
(Peter Grabowski is a Senior University Teacher in ScHARR and is Programme Lead for the MSc in Human Nutrition. He collaboratively developed the above project during a secondment as a Faculty Officer for Learning and Teaching.)
M.Ed. Graduation
In January, Emma Hock graduated from the School of Education with an MEd in Teaching and Learning in Higher education. For her dissertation, she examined the impact of a new problem-based learning (PBL) module on the integration of teaching and research in a research-led department at a research-based institution, through interviews with staff and students on the module. Her findings revealed that the module gave students an insight into the research undertaken in the department, and further steps could be taken to make research-teaching integration more complete. In broad terms, participants highlighted a need to make research-teaching integration integral to both teaching and research, potentially involving a ‘win-win’ solution that respects the workloads of staff while also getting students more involved. She has presented her findings at the Learning and Teaching Scholarship Showcase at the University of Sheffield in November 2019 and June 2020.
(Emma Hock is a Senior Research Fellow in ScHARR. She leads on two MPH modules and is Deputy Programme Lead for the MSc International Health Technology Assessment, Pricing and Reimbursement.)
Filed under Uncategorized
Public Health Practice and Research Collaborative (PaRC) – Dr Annette Haywood, School of Health and Related Research (ScHARR)
 Dr Annette Haywood, Manager for the Public Health Practice and Research Collaborative (PaRC) (Yorkshire & Humber) recently blogged about her journey to becoming PaRC Manager.
Dr Annette Haywood, Manager for the Public Health Practice and Research Collaborative (PaRC) (Yorkshire & Humber) recently blogged about her journey to becoming PaRC Manager.
You can read more here:
See our short animation here:
Filed under Uncategorized
Experiencing MD Viva during lock-down and thinking about racism by Alicia Vedio
I am a postgraduate research student for a Doctorate of Medicine in Public Health, and a physician in the NHS. I started part time PGR studies in 2014 in the School of Health and Related Research (ScHARR) at The University of Sheffield, studying the role that healthcare practitioners have in access to healthcare and submitted my thesis early in January 2020.
My viva was initially planned for March 2020, but the university workers’ strikes, and later COVID 19, delayed this. It was finally arranged for the end of April during the lockdown in the UK. Having a viva during lockdown meant this had to be online and I did not know how would this affect the experience. I had a mock viva using Blackboard Collaborate with both my supervisors that was really useful but I noticed my connection was not strong due to being far from the modem at home. I made sure that on the day of the viva I was in my dining room where the modem is and asked everyone at home to find something to do so, as not to be interrupted – not an easy task during lock-down but it worked well, and I felt more relaxed!
It was a relief that the experience was enjoyable mainly because both my examiners were as interested in the subject of inequalities in access to health care as I am and I was pleased to receive some useful and also complimentary feedback. But of course, it was not all positive. Before the viva, I knew there was a significant gap in my thesis and I wanted to draw attention to it by naming it here. The gap was a lack of discussion of racism theory. I had been made aware of this and had been expecting to receive comments about this in the viva feedback. I did. It was not easy to realise that I had such a serious blind spot and that perhaps I, even if unwittingly, had avoided entering into a deeper analysis and discussion of the subject of racialisation and racism within health care. I really hope and expect that my experience will resonate with other researchers. The many discussions and meetings I attended that reflected the work of the Health Equity and Inclusion theme team made it easier to direct the work I needed to do.
Since my viva, I have learnt a lot about racism theory, and not only about academic work in relation to health care related to my viva feedback. A month after my viva, George Floyd was brutally murdered in the US because he was black – one of a long line of shocking murders of people of colour that has been happening for centuries – and that it was made globally public due to being shared widely within social networks. It sparked a strong worldwide response and has also highlighted some really important resources on the work white people need to do to build a society that is fair to people of colour by dismantling racism. Systemic and structural/organisational racism are useful concepts that help to research and discuss barriers of access to health care services. Understanding structural racism is important but I (we) also need to work on our own blind spots to generate real changes in our lives and where we work. Most importantly, personal realisations are hard to confront. Knowing that I grew up in a white-dominated society with racist structures, organisations, and daily messages and education makes clear why I failed to name such an important issue but is deeply uncomfortable. My only consolation is that I am one of millions of white people in this society with the same problem to tackle. Intent and impact comes to mind, and impact is what we need to focus on. These two concepts refer to how we need to look at the effects of our actions and of the society structures. Intent may be positive but this is not relevant to the detrimental impact it has.
In conclusion, I have learnt that we can only work towards anti-racism and, for me, incorporating this in my thesis is only one of many steps. However, seeing racism and naming racism, is essential for in-depth change and this is why I wanted to tell my story here. Like everyone, my identity is an important part of my life. I am white, despite being of mixed indigenous, Black and Jewish descent, but I am mostly from white-mixed European descent, and I am myself a migrant descending from migrants. My own life experience and that of my ancestors impacted who I am today.
I now realise that the deconstruction required to eliminate racism is life-long work regardless of age and it is essential. In my study and work I look into addressing the role practitioners have in facilitating or hindering access to healthcare for a particular population. I explored the impact myself and other practitioners have, approaching it with an inequalities lens trying to address the imbalance of power between practitioner and individuals. My work now is to link societal, structural and personal racism to understand its role in creating barriers, in influencing personal development and in impacting the work of the NHS.
I also wanted to share some of the excellent resources I have encountered in my search for understanding.
“The Great Unlearn” and “Do the Work” by Rachel Cargle provides many examples of how white supremacy and white privilege work and gives frameworks that help examine how organisations can respond to this problem.
“Me and White Supremacy” by Layla Saad names many of the barriers to dismantling racism and these are well structured and clearly explained. You can also find her in YouTube describing her book in four steps.
I particularly found “Mindful of Race” a book by Ruth King (2018) helpful- this is a journey through an understanding of racism with a mindfulness framework and helps understand this oppression more clearly. Ruth King uses Buddhist concepts and shares her own experiences in helping organisations become more inclusive, diverse and anti-racist.
There are many more anti-racist resources available; these are some of the ones that have helped me greatly. I would encourage you to explore these or other resources to ensure that, together, we have a collective impact on dismantling societal and structural racism.
Alicia Vedio
Infectious Diseases Physician, Postgraduate Researcher Public Health, School of Health and Related Research, The University of Sheffield – abvedio1@sheffield.ac.uk
Publications:
https://onlinelibrary.wiley.com/doi/full/10.1111/jvh.12673
https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-017- 4796-4
Filed under Uncategorized
How to conduct a stakeholder workshop virtually during a global health crisis by Naomi Gibbs
Background: I am a ScHARR PhD student, approaching my final year. My academic background is in economics and health economics, but I also have 10 years work experience in the third sector. Alcohol poses a significant public health problem in South Africa and there is real interest in effective policy solutions. I am trying to  contribute evidence via building a health economic model of a minimum unit price, with a focus on how the policy might affect groups of people differently, for example rich vs poor. A minimum unit price basically removes the cheapest alcohol from the market, such as the wine pictured here which is £1.16 per litre (although this is far from the cheapest alcohol available). Stakeholder engagement is key to make sure the modelling fits with the context. It has allowed me to see the problem through a new lens and given me the opportunity to listen to diverse voices; something I really enjoy.
contribute evidence via building a health economic model of a minimum unit price, with a focus on how the policy might affect groups of people differently, for example rich vs poor. A minimum unit price basically removes the cheapest alcohol from the market, such as the wine pictured here which is £1.16 per litre (although this is far from the cheapest alcohol available). Stakeholder engagement is key to make sure the modelling fits with the context. It has allowed me to see the problem through a new lens and given me the opportunity to listen to diverse voices; something I really enjoy.
My stakeholders began with scoping interviews in August 2019 and then, last November, I went to South Africa to deliver the first of three planned workshops. In this initial workshop I asked stakeholders to complete a mapping exercise of alcohol harm in South Africa. I then asked them to choose the specific pricing policy they would like modelled, for example a change to taxation levels or structure, minimum prices, ban on discounting or any other pricing policy. They chose minimum pricing. They then highlighted subgroups of interest (women, poor, heavy drinkers, different age groups) and health outcomes they wanted included in the model. Because of this workshop I discovered that violence and HIV were critical to include in the alcohol model. My second workshop aimed to inform them of my progress so far and seek feedback on assumptions and critical modelling decisions, for example do we expect drinkers to switch to home brewing when facing a price increase and if so, to what extent. I also wanted to use it to present some preliminary results and discuss communication strategies. I was ready to go to deliver the workshop face to face in Cape Town, South Africa in May 2020 when Covid-19 hit. Since I had a space saved in everyone’s diaries, and with no possible way of knowing when I, or my stakeholders, would be able to travel and meet again, I decided to deliver the workshop online. This involved a significant rewrite of the workshop material, it had to be shorter and clearer. I had to think about how I would gather stakeholder feedback in an online context. I also needed to learn about the software as I didn’t want incompetence with the technology to be a distraction.
I was pleased with the outcome of my online workshop; it was well attended, I received positive feedback on the content and format and, crucially, I got what I needed to shape the next stage of my research including suggestions for data sources, choice of assumptions, direction for what other health outcomes should be included in the model, advice on how to present results and a collective communication strategy for the final results. Part of my success was due to circumstance; the sale of alcohol had been banned entirely during lockdown in South Africa, making it a hot policy topic, and encouraging attendance. Additionally, people were far more used to, and competent at, online meetings as they had all been forced into it by Covid-19 restrictions. Nevertheless, I spent a lot of time and effort carefully preparing and planning the webinar which was critical to the smooth running on the day.

Despite the success I would like to mention one pitfall from running the workshop online. My experience was that community groups found it harder to engage than policy makers and academics. They had the worst internet connections and computers and sometimes couldn’t even find a physical space to facilitate their participation. This was a loss and although I have tried to follow it up with them individually, I have struggled to get the level of engagement I got when I was in a room with them in November. For my final workshop/webinar I will ask these specific stakeholders if there is anything I can do to facilitate their engagement, perhaps sending hard copies of materials in advance with stamped addressed envelopes for feedback, I don’t know but I will ask. If you are reading this and have an idea please let me know. It is important to the research to make it as inclusive as possible.
I also benefited massively from the input of lots of different people. The support is there if you ask. Learning Technologists, information governance, ethics committees, supervisors, peers, family and friends. Don’t think you have to do it all by yourself. I am very grateful to the six peers who sacrificed two hours of their time to go through all the material and provide such useful advice, it would not have been half as good without them! So I thought I would share with you a list of simple tasks that helped me organise my webinar, maybe it will help you in conducting your own online workshop. I hope so.
On that note if you want any further help or advice please do feel free to get in touch.
Naomi Gibbs
n.gibbs@sheffield.ac.uk
Instructions:
- Consult your institution’s information governance team about data management before you choose your platform and submit your ethics application.
- Consult a learning technologist within your institution and ask them to teach you how to use the software (I used blackboard collaborate and enjoyed it as it felt like a very controlled environment, the slides are uploaded in advance, the live polls and chat box are very simple).
- Rewrite your consent forms online (I used google forms as this complied with information governance rules).
- On receipt of ethical approval invite your recipients to your event. Provide them with a link to the online consent form and the participant information sheet. Tell participants they will not receive a link to the event until they have completed the consent form.
- Plan your material, make it as short as possible (2 hours maximum) and make it interactive. Blackboard collaborate allows you to use live polls. Although these are a bit clunky, as you can’t pre-load them, they are invaluable at making you feel connected to your stakeholders and keeping their attention away from their inbox.
- Use online short questionnaires to gather written feedback throughout the online workshop. You can post the link into the chatbox and participants can simply click through. Split the material into 10 minute chunks. This will break the session up nicely for participants between listening and providing feedback.
- Schedule a tea break for half way. This is really important for you but also for your participants.
- Pilot your material a lot. Test it with anybody who will listen, family or friends first, then upgrade to peers. Make sure you also complete a technical run-through with your least technologically competent stakeholders (if you know who they are).
- Give time at the beginning to let people introduce themselves and say what their interest in the topic is. At the end, give people an opportunity to offer one key point about the research, however also give them the option to pass. Sometimes the comments you get during this period are as important as all the written feedback. I ensured this ran smoothly by naming people one by one and asking them to un-mute themselves. Being a clear facilitator is important here.
- Remember to record your webinar so you can listen to it again.
Filed under Uncategorized